Drs. Lonnie & Paul Zeltzer
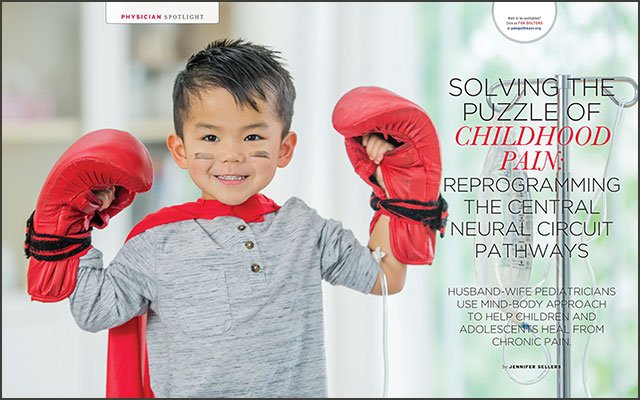
Solving the Puzzle of Childhood Pain: Reprogramming the central neural circuit pathways
“You can’t be someone who likes immediate gratification, and there aren’t usually any quick fixes.”
That’s a fact that Lonnie Zeltzer, MD, establishes right away. She’s been treating children and adolescents for the past 30 years and has had a pediatric pain research program for just as long. She and her husband, Paul Zeltzer, MD, run Whole Child LA in Los Angeles, the first-of-its-kind independent, integrative mind-body clinic, and together they wrote a book on chronic pain in young people called Pain in Children & Young Adults: The Journey Back to Normal.
In her practice, Dr. Lonnie Zeltzer sees patients who have failed to receive answers anywhere else. Often, she finds herself putting together the puzzle pieces from all the various specialists the children have visited, as well as their full history, birth history, family history and trauma history.
“I always call the kids and their families ‘onion families,’” she says. “As soon as we peel away one layer, we find another and another. In the process of talking with them, more and more things are revealed.”
Dr. Zeltzer says she does this to not only get at the root of what’s causing the child’s pain, but also to create a very targeted and specific treatment plan that takes into account the whole child.
Mind-Body Connection
When it comes to pediatric pain, research into the mind-body connection has been opening up doors for better understanding and treatment options. Dr. Zeltzer, who has been studying the mind-body connection for many years, uses this knowledge to help her patients and their families change the way they think about pain.
“In our research now, we’re doing functional and structural brain imaging,” she says. “We’re learning that kids with IBS, for example, have certain pathologic pain pathways that are set up. We’ve known this about adults for a few years, but in kids, there’s more of an opportunity to change those pathways. So kids with fibromyalgia, for example, don’t have to have lifelong fibromyalgia. There’s a lot of room to change that central control station that controls chronic pain.”
The Zeltzers treat a wide variety of chronic pain disorders in children. The most common they see are migraine headaches, irritable bowel syndrome (IBS), complex regional pain syndrome (CRPS) and fibromyalgia. However, all of the pain disorders come back to the brain, says Dr. Zeltzer.
“A child may have CRPS that originates from a foot injury, but controlling that pain is brain control, not foot control,” she says.
And that pain can lead to more pain. “When the child has pain, they’re not sleeping,” she continues. “And when they’re not sleeping, that adds further pain because the brain doesn’t have time at night to retrain those neural circuits.”
This is why psychological interventions are a big part of how the Zeltzers treat chronic pain in children. There are strategies that can help kids reprogram that pathologic brain circuit, says Dr. Zeltzer, whose early research grants from the National Institutes of Health were on the topic of using imagery to turn off pain.
“The more research there is in brain imaging in kids, the more we’re learning about the biologic consequences of psychological factors when it comes to pain circuitry in the brain,” she explains. “What’s exciting is that we’re getting to learn how different psychological interventions actually change pathological circuits to reprogram the brain.”
This mind-body connection is why Dr. Zeltzer advises not to keep asking your child if he or she is in pain. It actually reinforces it and makes the pain worse. Likewise, what you feed the brain can improve a child’s pain.
People may wonder how talking to a psychologist physically affects the body, improving symptoms like abdominal pain or muscle pain. The key is in specific strategies developed by the psychologists and other practitioners.
“It’s not just talking; there are very specific strategies that psychologists learn to help kids reprogram that circuit, and it works better than any medication you could come up with,” says Dr. Zeltzer. “When a child works with a psychologist doing biofeedback, imagery work or whatever works for them, they’re reprogramming that central neural circuit to get rid of that top-down pain-control system.”
Finding a Coach
While the Zeltzers’ mind-body methods have proven successful, the child and adolescent patients treated at Whole Child LA sometimes must travel a long road to achieve success. First, they’re typically referred to a specialist by their pediatrician; a child with migraines will end up in a neurologist’s office, or a child with musculoskeletal pain will be sent to a rheumatologist’s office. If the medications or treatments they receive from these physicians fail, the children and their families will often be left with no hope, bouncing from sub-specialist to sub-specialist until they finally find their way to Whole Child LA.
“We see the children who have not been helped by more traditional means,” says Dr. Zeltzer. “A lot of kids have seen 14 or more subspecialists and have undergone many highly costly evaluations before coming to us. There are a lot of pathways to us, but now there are many pediatricians who are automatically referring to us because we’ve seen patients of theirs before.”
According to Dr. Zeltzer, the patients have often seen very talented physicians, but each specialist is only looking at the organ system they have expertise in. To really tie everything together, the patient needs to be looked at as a whole, bringing that mind-body connection together.
The Zeltzers realize not all families are able to travel to receive their services. The good news, however, is that there are more and more pediatric pain clinics around the country, often associated with major medical centers. In the back of their book, the Zeltzers offer a contact list of integrative pediatric pain clinics that existed at the time of publishing. Dr. Zeltzer also recommends checking with the American Pain Society for a list of centers.
“Even if it’s a bit far, it’s worth it to visit the pediatric pain center nearest you for at least a consult,” she says. “We see kids from all over the country, and often it’s so that we can evaluate the child and provide the family with a report they can take back to the pediatrician and psychologist on their local team.
“It’s a team approach,” she continues. “It’s not just going to a psychologist or an acupuncturist or here or there. If they don’t have a pediatric pain specialist to work with they need their primary physician or pediatrician coordinating all the care. They need someone coaching the team. If they see lots of different clinicians and nobody’s talking with each other, they’re going to be getting a thousand different messages about what is wrong from each different provider. I say to parents: don’t go to 5,000 subspecialists and acupuncturists and physical therapists. You need a coordinated team, and you need a coach. The parent should not be the coach.”
Climbing the Mountain
Dr. Zeltzer says that by the time a family reaches them, it’s like they’re at the bottom of a mountain and can’t imagine climbing it. She says they often want a pill that gets them to the top, but it doesn’t work way.
“There’s no instant gratification in this, but over time the kids do get better and it’s very exciting for them, and very exciting for us,” she says.
Climbing the mountain involves an integrative, whole-child approach. “A lot of it is helping them understand the contributors to pain, what’s keeping the pain going, what’s making it worse and what’s the pathway out,” says Dr. Zeltzer.
This pathway out sometimes involves medication, but it also includes other methods, such as good sleep, exercise, physical therapy, integrative treatments and the all-important mind-body methods.
As the treatments take hold, children will first see improvement in functioning.
“They’ll start functioning more before they say they feel better,” says Dr. Zeltzer. “They’ll be able to do more and more. And of course they may be using muscles they haven’t used for a long time, so they may even have a little more pain. The pain is the last to go, so look at pain, not verbiage. They may be saying they’re still in pain, but now they’re able to go to school or work or activities with their friends.”
While Whole Child LA treats a patient population that seems destined for a lifetime of chronic pain, they see amazing success rates. Dr. Zeltzer estimates that around 80 percent of their patients improve.
“We see the worst of the worst—those who have failed in specialty care,” she says. “Yet, mind-body methods that address pain thoroughly and holistically can bring relief to even these children.”
As for parents’ job in all this, Dr. Zeltzer recommends that parents appreciate the suffering and take it seriously.
“Just be supportive and encouraging, help your child gradually be able to function,” she says. “Believe your child. If your child is hurting, it doesn’t matter if a doctor can’t find anything structurally wrong. A lot of pain is just neuro-signaling, and you aren’t going to see that in a usual test. ”
PainPathways Magazine
PainPathways is the first, only and ultimate pain magazine. First published in spring 2008, PainPathways is the culmination of the vision of Richard L. Rauck, MD, to provide a shared resource for people living with and caring for others in pain. This quarterly resource not only provides in-depth information on current treatments, therapies and research studies but also connects people who live with pain, both personally and professionally.
View All By PainPathways