Pain Triangle – Understanding Causes And Solutions

The ‘pain triangle’ paradigm provides patients with a lot of information and potential avenues for healing despite its seeming simplicity.
However, there are many competing ideas and models that make it difficult, if not impossible, for persons with chronic pain to make sense of their experiences.
How Can Pain Triangle Affect Those Who Experience Pain?
There are many competing ideas and models that make it difficult, if not impossible, for persons with chronic pain to make sense of their experiences.

However, the ‘pain triangle’ paradigm provides patients with a lot of information and potential avenues for healing despite its seeming simplicity.
If you want to go past your suffering, it helps to have a firm grasp on what causes it. You can handle a situation considerably more effective if you have a thorough understanding of its components.
In order to effectively manage chronic pain, it is important to have access to the information you need. However, it can be difficult to sort among the available research and theories on pain.
In this essay, we’ll try to break down the components of the pain triangle, a popular model for understanding these kinds of problems. When applied to chronic pain, this approach can lead to improved coping strategies and a deeper comprehension of the condition.
When pain persists for more than three months, medical professionals use the term “chronic pain.” For those who experience it, the resulting bewilderment and isolation can be devastating.
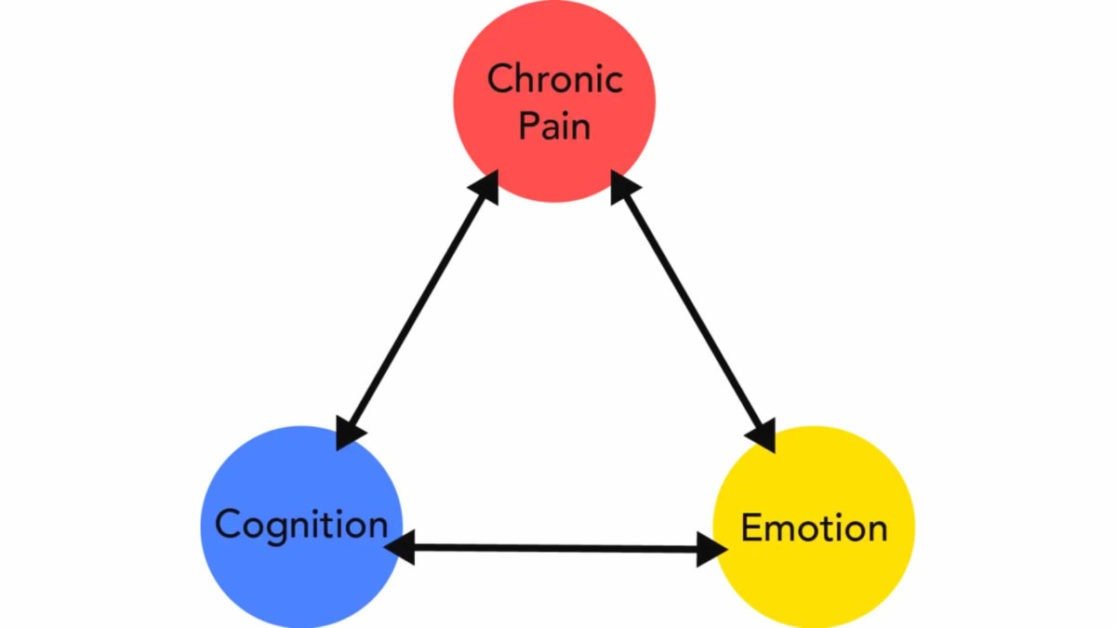
A pain triangle is a useful tool for depicting the interplay between pain and other aspects of our being.
Pain thought, and feel make up the three sides of the pain triangle. Chronic pain is the apex of a triangle with cognition (one’s thoughts and beliefs about the pain) and emotion (one’s feelings about the pain) occupying the two base points.
The three vertices of this triangle represent the interconnected effects and difficulties that chronic pain has on both mental and emotional processes.
Pain Triangle – Chronic Pain
Problems with concentration, memory, attention, and executive functioning are just some of the cognitive difficulties that may arise as a result of living with chronic pain. Alterations in one’s state of mind can also amplify and intensify the experience of pain.

Journal of Pain and Symptom Management studies indicated that 42% of patients with chronic pain and no history of brain damage reported at least one cognitive problem.
This is true even if it is unclear whether cognitive difficulties will emerge early on in the course of people with chronic pain or much later on.
The study goes on to detail the potential causes of these cognitive complaints, including neurological abnormalities, medication for pain, the experience of pain, an obsession with injury or illness, sleep deprivation, stressful life events, and other emotional variables.
Because there are so many different factors that could contribute to cognitive impairment, it is essential to have a close relationship with your treating physician or another medical expert. In this way, any problems that do arise can be rapidly identified and addressed once they are identified.
Feelings of despair, panic, wrath, irritation, and helplessness are all common emotional responses to chronic pain. All of these negative emotions can increase a person’s sense of pain, whereas optimistic perspectives have been demonstrated to lessen it.
Patients with chronic pain face a range of psychological challenges, from moderate emotions of self-esteem concerns and insecurity to considerably more significant problems, including self-harm and even suicide.
There is a wide range of emotions that can accompany chronic pain, from worry about future pain flare-ups to outright terror of the agony getting even worse.
The negative narratives we tell ourselves, such as “Why is this happening to me?” and “How can I ever cope with this?” are widespread, and they may have a devastating effect on our emotional and mental health if they persist.
Pain Triangle – Chronic Pain Cognitive And Emotional
Cognitive and emotional difficulties can have far-reaching consequences on patients’ daily lives. When mentally challenged, it’s common to have a decline in working memory and productivity.
Additionally, when experiencing emotional distress, one may unwittingly initiate problems in their relationships, which, if left unaddressed, can lead to social withdrawal, loneliness, and isolation.
The cognitive and emotional difficulties experienced by those with chronic pain tend to repeat themselves. Pain flare-ups exacerbate mental and emotional difficulties.
If the discomfort subsides, these other problems should go away, too. If you feel that you’re stuck in a cycle, you should know that there are ways out.
Spending time with loved ones, engaging in religious or spiritual activities, meditating, joining a chronic pain support group, taking up a new activity, keeping a journal, and adopting a more optimistic outlook are all ways to help alleviate suffering.
Dr. Edward Zelman
Dr. Edward Zelman is a distinguished and highly respected medical professional who has dedicated his career to the field of general medicine. With a profound commitment to patient care and a wealth of knowledge acquired over decades of practice, Dr. Zelman has earned a reputation as a trusted healthcare provider in his community. With a career defined by excellence and an unwavering commitment to the betterment of his patients and the broader community, Dr. Edward Zelman stands as a pillar of the medical field, dedicated to the principles of healing and compassionate care. At present, Dr. Edward Zelman is researching safe and effective natural remedies that can restore as well as maintain the youthful functioning of the body.
View All By Dr. Edward