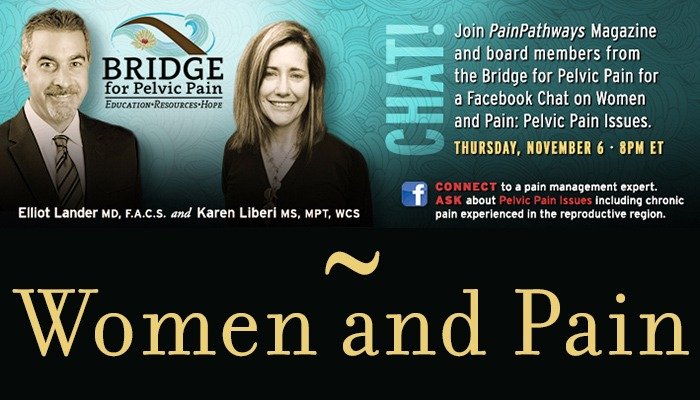
Pelvic Pain Facebook Chat
Understanding Chronic Pelvic Pain
Transcript Highlights
Dr. Lander & Karen Liberi, MS, MPT, WCS
November 6, 2014
Welcome! Thank you for joining us today for “Women and Pain: Pelvic Issues Including Chronic Pain Experienced in the Reproductive Region”. This Facebook chat will be hosted by Dr. Elliot Lander and Karen Liberi, MPT of Bridge for Pelvic Pain and will cover topics such as:
– What is pelvic inflammatory disease?
– Various causes of pelvic pain including IBS, urinary tract infections, Interstitial Cystitis
– Pelvic conditions, such as pelvic organ prolapse
– Pain during sexual intercourse
– Treatments for pelvic pain
– And more
Dr. Lander has served as Chief of Urology at Eisenhower Medical Center and Chief of Surgery at John F. Kennedy Hospital. He has been on staff at Eisenhower Medical Center for eighteen years and is also an Expert Reviewer in Urology for the California Medical Board.
Karen Liberi, MPT is one of only 150 physical therapists in the United States with the designation of Women’s Health Clinical Specialists. She is committed to educating health care providers and community members alike about the importance of addressing the often-neglected area of the body between the belly button and the upper thighs.
Now, please join us in welcoming Dr. Lander and Ms. Liberi!
Dr. Lander: Hello, this is Dr. Lander, happy to be here.
Karen Liberi: Thank you so much for inviting me to this chat. I am very excited to be here.
Reader: Can Botox injections help with pain I bladder or PFD?
Dr. Lander: Botox is primarily for overactive bladder but some patients report improvement in pain.
Reader: My husband and I both have IC and severe pelvic pain, but doctors keep putting us off. Prostate issues are our concern.
Karen Liberi: If your husband has non-bacterial prostatitis, then physical therapy can be
useful in minimizing the tension surrounding the prostate to minimize his pain. Relaxation
breathing for both of you for belly expansion and pelvic floor relaxation can take some
tension away from the bladder to help “take the edge off.” One really great resource can
be Dustienne Miller’s, “Yoga for Pelvic Pain” to allow for relaxation and quieting our “fight or flight” nervous system to assist with managing your pain.
Reader: I think the reason people use the term “down there” is that it’s so hard to even determine where your pain is actually coming from. Is it urological, vaginal, the bladder, and the stomach? Where does one start when beginning to deal with pain in this generalized region?
Karen Liberi: It can be difficult as there are urologists, gynecologists, colo-rectal doctors. I think that an urogynecologist would be a good start as they can address the various components of “pain down there”. Look for the new DVD coming out in early 2015 titled, “Healing the Pain Down There“, that can be used as a great resource as well.
Reader: Seven years ago I had a colposcopy done after they found a possibility of precancerous cells. It came back negative. Since that procedure, I have had monthly UTIs, bladder infections and rarely, but a few, yeast infections. I am 25 now and unfortunately my conditions have worsened. I am afraid to go pee, because I’m afraid to get the UTI feeling and I can’t have sex because my bladder is in constant pain, which hurts more during sex. It’s a terrible thing to go through with my soon to be husband. I have become depressed over this because my sex life and daily lifestyle used to be normal. I have seen urologists and OB-GYNs, and my primary care. One thinks I have IC, but is not 100% certain. What do you think it could be or what should I do?
Karen Liberi: Have your bladder infections been confirmed? Have you had a “work up” for IC? UTI feeling can come from muscular tension around the urethra? Has your doctor tried you on Pyridium (takes away urethral pain if pain is coming from the urethra)? If you feel you can’t have sex, this may be related to “anticipatory gripping reflex” as your muscles are tightening in anticipation of pain. There are positions to avoid deeper penetration to minimize pressure and pain at the bladder. I would recommend seeing a women’s health physical therapist to help you navigate what is happening with you. Here is a link to help you find one. There is a good book that addresses how your pelvic pain impacts your relationship, “Secret Suffering”. Also, “Pelvic Pain Solutions” actually has a heating pad that you CAN wear around town. Hopefully, these suggestions can help you get started on a successful path of healing!
Dr. Lander: You need a good urological evaluation including physical exam and cystoscopy to check the integrity of the bladder lining. You need to find out if you have positive cultures with your UTIs or are you just feeling like it’s a UTI, which may be the beginnings of IC. Ask your urologist about a low dose suppressive antibiotic for a three- to six-month period.
Reader: Can pelvic dysfunction masquerade as sacroiliac joint pain…radiating across the buttocks? Do you have any recommendations for physical therapists and pelvic pain departments in North Carolina?
Dr. Lander: Some pelvic pain is felt in the back, but it’s usually part of a pain spectrum that extends to other areas as well. Isolated sacro-iliac pain can be many things including arthritis, certain auto-immune conditions, muscle spasm, disk pain, etc. Some patients are responding to Botox injections into the bladder wall. They can be performed in the office under local anesthesia or under sedation. Safety appears to be reasonable but some patients have difficulty voiding afterwards which is usually temporary.
Links shared: Carolinas Healthcare – Pelvic Health.
Reader: I have been diagnosed with Pelvic Floor Dysfunction in which I have a lot of pelvic pain. The worst pain for me to deal with is a spasm type pain that comes from the vagina area to my labia minora which causes it to swell up and has caused it to enlarge on the right side. Is this typical of pelvic pain? I also get a lot of UTIs. I have gone to PT and it has helped but not with the labia pain that much. There are times I feel like I have been in a car wreck and the pelvis was damaged the most. Another question is– can a herniated disc that is pressing on nerves of the L4 and L5 cause pelvic pain? I have pretty much become invalid since June the 16 when this all began in a blink of an eye.
Dr. Lander: The UTI may not be related to the pelvic pain. Those require a formal workup including cystoscopy and possible imaging, and urine testing. The pudendal nerve has a branch that innervates the labia and you may have damage on the right side. Your physician should be able to evaluate that with a MRI and physical exam. Karen can discuss many interventions that are effective for pelvic floor dysfunction.
Karen Liberi: The swelling may be coming from a lymphatic blockage, this is not typical, but certainly there can be a reasonable explanation for this. Sometimes if manual lymphatic drainage is added to the PT treatment – this may be helpful for the labia as well. Usually S234 is where pain to the pelvic floor comes from (pudendal nerve).
PainPathways Magazine: This resource from Dr. Lander may be helpful: The IC Optimist.
Reader: Hi, I have a mass the size of an orange and growing. I’ve been to two OBGYNs and two cancer doctors the mass is on my ovaries. No one wants to do surgery because I’m overweight. One cancer doctor said he’d do surgery if I agreed to have gastric bypass surgery first. I’m in a lot of pain and I’m at the end of my rope.
Dr. Lander: Your experts apparently have concurred with resection of the mass but sometimes physicians will defer surgery that is not emergent if a person’s body mass index is high since surgical risk goes up dramatically in such cases. Make sure your surgeon is well versed in the latest laparoscopic techniques.
Reader: Can IC/PFD cause erectile issues in men? And, can PT help, or other treatments help?
Dr. Lander: From Karen: PFD can absolutely cause erectile issues in men. PT can be very valuable in helping this. Here are resources you can use to find a pelvic floor therapist.
Section on Women’s Health
Herman & Wallace Pelvic Rehabilitation Institute
Reader: I’ve been able to maintain my IC with water and diet. I have minimal pain compared to others I’ve read about, so I feel really fortunate. Now my 26-year-old son is having issues. Do you think IC can be hereditary or have there been any studies in that area?
Dr. Lander: Studies of mothers, daughters, and twins who have IC suggest a hereditary risk factor but no specific gene has been identified. Your son will need a full work-up to evaluate other causes of pelvic pain but men do get IC and his physician should look specifically for it (the ratio of women to men with IC is approx 10 to 1).
Reader: Where is a good place to start when trying to get pelvic pain diagnosed?
Karen Liberi: An urogynecologist would be a great place to start.
Reader: Since no one can pinpoint exactly what cause the brain to have nerve ending issues that contribute to chronic pain—– is it possible for the brain/nerves or whatever to heal and the chronic pain STOP?
Karen Liberi: There is tremendous research coming out of Australia on the brain’s role in chronic pelvic pain. Look into the NOI group as you will find lots of great information.There is a great new book called “Why Pelvic Pain Hurts”, which discusses the brain’s role in chronic pain. You can also Google Lorimer Mosely and pain videos as these can be valuable to you as well.
Reader: A doctor’s procedure gave me severe pelvic pain for about a decade. It finally lessened – and I chose to never have a pap smear again due to the severe pain the procedure induced. In January, my regular gyno tried to give me a pap and by the time I yelled “bloody murder”, the damage had been done – and I was back to square one. I won’t see a doctor or PT, but have chosen self-care. I’m slowly improving. Any self-care ideas or advice?
Dr. Lander: This sounds like the procedure resulted in a flare of pain, which may be related to pelvic floor spasm. Karen may be helpful here.
Reader: I’ve been told I may have interstitial cystitis. What is it and what are the treatments? Have there been any recent discoveries or treatments?
Dr. Lander: Learn about pentosan in liposomes for instillation.
Karen Liberi: A great website; theIC Network.
Reader: What area of IC is helping the most in your stem cell therapy, pain, burning, frequency, etc… Also many women who have tried stem cell therapy at your clinic are also doing other treatments simultaneously. If this is the case, how does one really know what therapy is working??
Dr. Lander: Some patients have a better response to pain but overall the bladder symptoms do the best. Most of our patients have tried everything they know but sometimes it is difficult to sort out what factors are most beneficial.
PainPathways Magazine: Other great resources: “Ending Female Pain” and “Secret Suffering“.
Reader: I’ve had the IC diagnosis six months ago, although I have treated urinary infections almost 20 years. I have done lots of exams and after the third specialist I consulted, I have had the following advice: to urinate every two hours, no diet, no medications, but I keep feeling horrible pain. I almost have no sexual relationship and I am depressed. I don’t know what to do, since I’ve consulted the major specialists on this area in Brazil. I really want to know a way to have my life back.
Karen Liberi: Have these bladder infections been confirmed? Sometimes IC or urethral syndrome can mimic a urinary tract infection; however, there is no sign of an infection upon testing. Knowing more about the exams performed would help me better to help you move in the right direction for help. Knowing specifically WHERE your pain is would be helpful. (Lower, central abdomen, urethra and/or vaginal). Understanding your pain better can help to feel less depressed about it. Depending on where the pain is coming from, strategies can be used to help to return to sex.
Resources such as “Bridge for Pelvic Pain”, Wendy Cohan’s book, “The Better Bladder Book”, the soon to be released DVD, “Healing the Pain Down There”, as well as Isa Herrera’s book “Ending Female Pain” could all be good starts in getting some answers and sharing the information you learn with your doctors. In terms of the dynamics of your relationship, the book “Secret Suffering” may be useful for you as well. Hope this helps to give you some direction on your journey to feeling better!
Reader: I have PFD and IC and Fibro I am now hurting with sciatic nerve pain. It goes into the buttock-area and down the back of my one leg. What will help this?
Karen Liberi: For the sciatica – generally a piriformis stretch can be helpful and sometimes lumbar extension exercises depending on where the nerve is being irritated along its path.
Reader: I’m a 28-year-old female whose had fibromyalgia, weight gain, and severe IBS the last 10 years. I thought my pelvic pain had to do with my monthly cycle, but an entire week after my cycle ended, I was in a lot of lower abdominal pain.
Karen Liberi: There are so many contributing factors to abdominal pain including hormonal influences (i.e surrounding your cycle) digestive influences as well as bladder influences and myofascial/muscular pain. Finding a good doctor and physical therapist can help you further determine the cause of your pain and therefore set you on a plan for improving your pain. There are a couple of books called, “Heal Pelvic Pain” and “Ending Female Pain” which have good educational components, as well as exercises that can be helpful. Relaxation breathing and Iyengar based yoga can be helpful.
Reader: I started menstruating at age of 12, and since then I go through severe pain during my cycle and before, too. Now at 41, my situation has been improved but sometimes it causes unbearable pain. I have defected spine since birth, at L5, I do not remember medical term, and arthritis too. After my son’s birth through caesarian section, I could not stand for long and had severe pain all the time in pelvic area. Many therapies were applied at last I used homeopathy, I feel better but still prone to either infection or have PMS and period pain. Any alternate therapy that you would suggest?
Karen Liberi: A good resource for you may be “The Hormone Cure” which may assist with pain stemming from hormonal fluctuations and will give you a direction on where to go to help with your pain.
Reader: How to test the pelvic floor for hyper/hypo tonicity – for women who do not have access to a pelvic floor specialist. Are there any external palpation techniques that exercise specialist (pre/postnatal) can teach our clients? Best exercises for hypotonicity? Best exercises for hypertonicity? How surrounding muscles might play a part in pelvic pain? What muscles should we focus on in regards to myofascial release for both hypo/hyper?
Karen Liberi: I would refer to the reference: Evidence-Based Physical Therapy Pelvic Floor.
Reader: Can you please explain sensory pain and why sounds and vibrations hurt? Also, the delayed pain response…
Karen Liberi: The NOI group has so many great answers to this question. . I will refer you there.
Reader: I’ve been getting Botox for about a year now. Every 3 months. 1st couple of times were just in the office (excruciating) I had both bladder & pelvic floor done. After those initial injections I’ve been in retention ever since. I go to PT once a week and do gentle yoga. My concern is what’s the next step if I cannot void on my own ever again? My uro-gynecologist will not do my bladder again. Only pelvic floor. I’ve gotten great relief so it’s worth it to me to cath all the time. I just wonder if there’s something I can do to get back to urinating on my own. Thanks!
Dr. Lander: It is very rare to be in retention for up to a year. Botox has occasionally been known to affect nerves for 6 to 8 months. Please ask your doctor to perform formal urodynamic studies to assess your nerves and muscles of the bladder and it may be prudent to not obtain any more Botox until this is resolved.
Reader: I had a cystoscopy done a few weeks ago and the doctor said my bladder could only hold 200 cc and then my blood vessels would start bursting; he said that it was severe! What are your thoughts on that?
Dr. Lander: I don’t know your history but it sounds like your doctor was working you up for IC. IC can result in scarring and loss of bladder compliance.
Reader: 7 years ago I had a colposcopy done after they found a possibility of pre-cancerous cells, it came back negative. Since that procedure, I have had monthly UTIS, bladder infections and rarely but a few yeast infections. I am 25 now and unfortunately my conditions have worsened. I am afraid to go pee, because I’m afraid to get the UTI feeling and I can’t have sex because my bladder is in constant pain, which hurts more during sex. It’s a terrible thing to go through with my soon to be husband. I have become depressed over this because my sex life and daily lifestyle used to be normal. ..I have seen urologist and OBGYN(s), and my primary care. One thinks I have IC but is not 100% certain. The pain in my bladder has left for a few days now, however I still can’t have sex and it’s now left me never wanting to have sex, I lost that feeling of wanting it…sadly I feel I’m too young for this. What do you think it could be or what should I do? I suffer from UTIs, bladder infections and now major bladder pain. Heating pad helps but I cant wear it around town… I now live my life in fear of that area and carry around UTI medication just in case, would love for everything to disappear.
Dr. Lander: One of the problems with recurrent UTI(s) is that each infection makes the bladder more susceptible to another infection often leading to non-stop problems. We occasionally use chronic suppression antibiotics. Certain antibiotics are less associated with yeast infections and are safe in low doses over extended time periods. Ask your urologist about that.
PainPathways Magazine: Another great website resource for women: The Echenberg Institute for Pelvic & Sexual Pain.
Reader: Will cannabis, in pill form, be allowed for IC pain?
Dr. Lander: There are some derivatives of cannabis that have few “cannabis” effects but more pain relief effects. They are being studied now.
Reader: Does a women’s age affect the success of the stem cell therapy for IC. Just concerned about the quantity of stem cells that you are able to obtain based on one’s age?
Dr. Lander: If you use stem cells from fat, they do not degrade in proliferation and differentiation potential (quality) with age or chronic disease like the bone marrow derived stem cells.
Reader: I have IC and many other problems. I have many female surgeries. Does all that weaken the bladder? Plus the scar tissue I have. (I’ve had a hysterectomy due to endo).
Karen Liberi: You would definitely benefit from a pelvic floor physical therapy evaluation. Here are some websites, also mentioned previously, to find a therapist near you.
Section on Women’s Health
Herman & Wallace Pelvic Rehabilitation Institute
Scar tissue can definitely impact the strength of the pelvic floor and support of the bladder.
The tension you hold from the pain from the IC can also weaken your muscles and decrease support of your bladder.
Reader: Dr. Lander, What area of IC is helping the most in your stem cell therapy, pain, burning, frequency, etc..? Also many women who have tried stem cell therapy at your clinic are also doing other treatments simultaneously. If this is the case, how does one really know what therapy is working??
Dr. Lander: Some patients have better response to pain but overall the bladder symptoms do the best. Most of our patients have tried everything they know but sometimes it is difficult to sort out what factors are most beneficial.
Reader: Dr. Lander, I had a full hysterectomy over 10 years ago. I have never had a pelvic exam since. Is there a need for one after a hysterectomy?
Dr. Lander: This summer, The American College of Physicians (the group that represents INTERNISTS, not GYNECOLOGISTS) published a recommendation stating that non-pregnant women who do not have specific complaints need not have a gynecologic exam. The American Congress of obstetricians and gynecologists still recommend yearly exams. The performance of a physical examination is a key part of an annual health assessment visit, and the components of that examination may vary depending on the patient’s age, risk factors, and physician preference. If the patient had a total hysterectomy and bilateral oophorectomy, some physicians may omit the exam.
Reader: I am dealing with constant chronic pain and extreme pressure in the lower pubic mons above the pubis symphysis area that does not respond to internal pelvic therapy release of trigger points in the vagina and levator ani. I do have IC. What are the options for dealing with pelvic neuralgia and nerve pain? Dr. Weiss, in San Francisco, has a pelvic pain center that exclusively deals just with pelvic pain. He believes pudendal nerve neuralgia and PNE are frequently undiagnosed conditions. Most docs seem to group pelvic pain under IC referred pain. Do you agree? Since I live in San Diego, are there docs in the Southern CA area that do trigger point injections and other modalities to deal with non specific pelvic pain?
Dr. Lander: I do not have a specific referral but you are correct to pursue pudendal neuralgia with trigger point injections since it may not just be IC referred pain.
PainPathways Magazine: We appreciate all of your thoughtful questions and our experts’ informative responses. This has been a great dialogue.
PainPathways Magazine: This is Amy North, editor of PainPathways Magazine. On behalf of Dr. Richard Rauck, we’d like to thank Dr. Lander, Karen Liberi and all those who participated in tonight’s chat! We are excited to offer this great forum for information and inspiration.
Have a good night everyone!
Professional and Individual subscriptions to
PainPathways Magazine
are available at velaharbor.com.
All information provided is for educational purposes only. Neither PainPathways nor their Facebook Chat hosts are responsible for a medical diagnosis. Individuals should seek a physician for evaluation and personalized treatment plan.
PainPathways Magazine
PainPathways is the first, only and ultimate pain magazine. First published in spring 2008, PainPathways is the culmination of the vision of Richard L. Rauck, MD, to provide a shared resource for people living with and caring for others in pain. This quarterly resource not only provides in-depth information on current treatments, therapies and research studies but also connects people who live with pain, both personally and professionally.
View All By PainPathways