David Lemaster
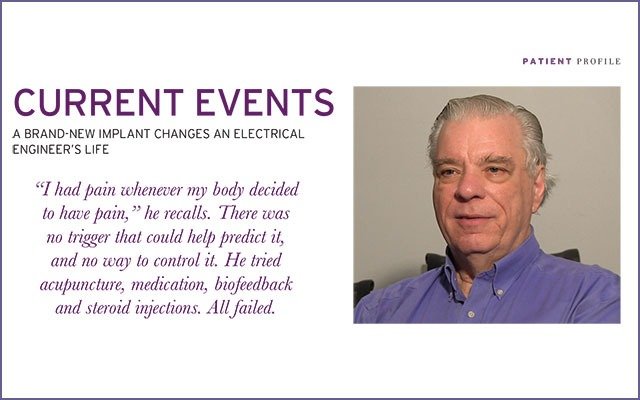
A brand-new implant changes an electrical engineer’s life
Acute arachnoiditis isn’t a disease you hear about every day. It’s a rare form of chronic pain caused by inflammation of a membrane around the spinal cord.
But David Lemaster, 70, is all too familiar with it. His arachnoiditis was brought on by a blood infection he contracted during surgery after a workplace fall. Lemaster, then 60, plummeted 12 feet from a ladder onto a concrete floor at the phone company he worked for. It was the second serious fall he’d had in his engineering career. He compressed three discs and suffered nerve root impingement.
He was being prepared for surgery, but excruciating pain caused him to go into atrial fibrillation (AFib), an irregular heartbeat that can lead to blood clots, stroke, heart failure and other serious ailments.
Lemaster, who lives in Willow Spring, North Carolina, ultimately had three surgeries as a result of the injuries he sustained in his fall, but arachnoiditis wasn’t diagnosed until after the third surgery.
As if all this weren’t enough, in response to his injuries his body also fused several vertebrae from the neck down. (He had seven vertebrae surgically fused—which is a corrective measure—but the others fused themselves.)
A little background: the absence of an intervertebral disc between two vertebrae is called a fusion. The bone connects directly to the bone above or below (or both) without the cushion of a spinal spacer.
Developed (as opposed to congenital) natural spinal fusions happen over time, usually due to degeneration or—in Lemaster’s case—injury. Consequences of organic fusions vary widely. Single-level natural fusions are rarely problematic, but multiple fusions can result in back or neck pain, which in some cases is debilitating.
For Lemaster, the painful consequences of the fall and multiple surgeries were nearly intolerable. He couldn’t work anymore. He could drive a car, but pain dictated his life.
“The nerves at the end of my spine are tangled up like spaghetti,” he says, describing his arachnoiditis. “When one nerve fires, it can go to any part of my body and cause pain.” Migraines and pain in the legs, hips and back … all can be traced back to arachnoiditis.
“I had pain whenever my body decided to have pain,” he recalls. There was no trigger that could help predict it, and no way to control it. He tried acupuncture, medication, biofeedback and steroid injections. All failed.
Lemaster was overdue for a little good fortune.
That came last February in the form of a newly FDA-approved implant. Duke University neurosurgeon Nandan Lad, MD, PhD, implanted the Nevro paddle HF10 near Lemaster’s spine, making him one of the first two patients in North Carolina to receive the device. More importantly, the procedure made Lemaster virtually pain free for the first time in eight years.
HF10 therapy has been used in Europe and Australia since 2011, but it didn’t get FDA approval until 2015. Lemaster can’t help but wonder what took the US so long to approve what he considers a miracle cure.
“It gave me 100 percent relief,” he says.
The device sends high-frequency electrical signals to calm the nerves that contribute to chronic pain. The surgeon puts electrical leads at the specific nerves causing pain and implants a separate battery pack to provide electrical current. The device, smaller than a deck of cards, takes just 30 minutes to charge, and Lemaster charges it every day. “The battery is so good,” he says, “it’s guaranteed to last ten years.”
Unlike other spinal cord stimulation therapies, HF10 can be left on during sleep and while driving. Plus, it isn’t likely to cause the tingling sensation—paresthesia—some patients complain about with typical spinal cord stimulation.
Why does HF10 work when other implants fail? It uses a higher frequency current. Patients who haven’t found relief through other treatments may find relief with this. Lemaster says, “It’s even better than advertised.”
Life is good again for David Lemaster. And for his wife, Barbara. “I’m more like the man she married,” Lemaster says. “When I was living with pain, I was not a nice person to live with.”
He now sleeps through the night—something pain hadn’t allowed him to do in years. He can mow the lawn again, although it tires him out. He’s considering getting a pacemaker and laughs about how he’d then have two pacemakers: one for his back and one for his heart.
Lemaster can get through his days and nights without debilitating pain. He’s still unable to work, but the magic of electricity—a field he knows well—is alive inside him.
PainPathways Magazine
PainPathways is the first, only and ultimate pain magazine. First published in spring 2008, PainPathways is the culmination of the vision of Richard L. Rauck, MD, to provide a shared resource for people living with and caring for others in pain. This quarterly resource not only provides in-depth information on current treatments, therapies and research studies but also connects people who live with pain, both personally and professionally.
View All By PainPathways