Tony Lawless
They thought it was “growing pains.”
When Tony Lawless developed pain in his left wrist at the age of 19, the first doctor he saw told him not to worry. The former high school football and lacrosse player had always been active, always healthy, and there didn’t seem to be any significant cause for alarm.
“But my wrist wouldn’t heal and things got worse,” Lawless recalls. “I ended up dropping out of college because [the pain got so bad] I couldn’t sit in the chair.”
Eventually, doctors diagnosed rheumatoid arthritis, and Lawless started a variety of treatment approaches. He recalls that he tried “all kinds of drugs and alternative therapies” to alleviate his pain, but doctors told him that he would likely be in a wheelchair by the time he was 25.
“It was good to figure out what it was, but on the four-hour ride back home, I was just in shock,” Lawless says. “But I also decided that I was not going to let this diagnosis take over my life. From that point on, I decided that I was going to do whatever I could do.”
Lawless continued with his “can-do” lifestyle until he began experiencing pain “from the top my head to my feet.” The debilitating pain continued to dramatically increase, prompting Lawless to think, “I’m just done.”
“I was in my room, not able to move, and my mom knocked on the door,” he says. “I told her that I was ready to die. She said, ‘Nope, that’s not going to happen.’ Then she helped me get up and get moving. It took two hours, but it made all the difference. From that moment on, I looked at things differently.”
In 1982, at age 22, Lawless decided to go to culinary school, and he says the decision saved his life. His doctors warned him that being on his feet all day would be challenging, but Lawless was determined. He started researching alternative treatment plans after experiencing side effects from the pain medicines that kept him functional. After living his life at a constant level of pain where a “2 day was a ‘yee ha!’ day,” he says he wanted a better quality of life. “Culinary school kept me moving,” he says, although it “hurt like hell.” A mix of prescription meds and alcohol dulled the pain, but he knew he needed to do something else if he wanted to live the kind of life he envisioned for himself. He found a medicine regimen that worked well, but then a sprained ankle in 1991 forced him to go back to square one.
“The arthritis got in there and trashed my ankle,” he says. “When I got out of the cast, we tried a lot of things to combat the pain. I had my ankle fused and hoped it would get rid of the pain; it did in my ankle, but then I developed a lot of pain in the front of my foot.” He’d been working 60-80 hours as a chef, running a catering company in Naples, Florida. He kept working through this entire period with intense pain. He began wearing a foam rocker-bottom boot, “dragging my foot around in it” for approximately five years.
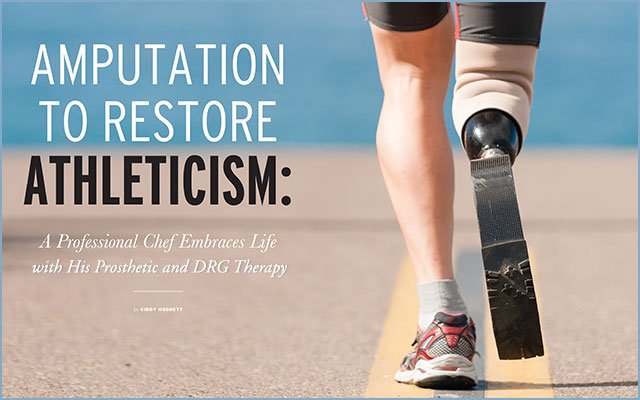
“I told the doctors they had to do something. They said that if I wanted to be mobile, I should think about an amputation,” he says. “So in 2000, on January 24, they cut off my leg below the knee, and I started hiking that summer and skiing that winter. The amputation gave me my life back.”

Lawless began skiing and started racing for and coaching a team that was part of a disabled recreation program. He says things were going great until a freak accident on the slopes left him with a broken femur and caused such substantial pain in his amputated leg that he was unable to walk easily, much less participate in physical activities. And this was on top of the constant nerve pain in his stump, not uncommon in amputees. He had tried surgery to fix the nerve pain, but it only made it worse.
“That was when I met Dr. Corey Hunter, a pain specialist with Ainsworth Institute,” Lawless says. “He suggested DRG (dorsal root ganglion) therapy, and it changed my life.”
DRG is a neurostimulation therapy that treats difficult-to-manage chronic pain isolated in a specific region of the lower body. A small device, implanted in a physician’s office, delivers electrical impulses to the dorsal root ganglia, and patients have the ability to adjust the strength of the stimulation. Lawless found relief immediately.
“After Dr. Hunter put in a trial [stimulator], I left his office to see how it worked and ended up doing a five-mile walk around Central Park.”
Dr. Hunter is also a patient educator on DRG therapy. He says that amputees often present pain challenges that are not easily addressed by traditional treatment approaches.
“Amputees are very motivated and often trying to find ways to get back to their lives,” Dr. Hunter says. “But amputation pain has a very weird distribution, and I compare traditional spinal cord stimulation to fishing with a net for the pain. By contrast, DRG is more like spear fishing. We can find where the pain is funneling in and focus the treatment to specific areas.
“Anthony was the fourth patient I implanted, and during the trial phase, he had 90 percent pain relief within hours,” Dr. Hunter continues. “When he came back after a week, he said, ‘This is what I want.’ He had nerve pain in his stump for five years, but now he is defying everything anyone might think about an amputee. He has few, if any, limitations, and is able to do everything he wants to do.”

Dr. Hunter says that DRG therapy has offered relief to patients with some of the most difficult pain presentations, including pelvic and knee pain—both difficult to treat with traditional methods. He also thinks DRG is an alternative to opioids.
“We are all very excited about the results from DRG therapy so far,” says Dr. Hunter. “Abbott [the company that offers DRG therapy] has done a fantastic job with public outreach, and this is an important advancement in the treatment of chronic pain.”
For Lawless, now two years into his DRG therapy, the results have been life changing, and he now spends time educating other amputees about the possibilities of a pain-free, active life with a prosthetic.
“Someone told me that we have a choice every day when we wake up—we can choose the path we want to walk, whether on nails or on moss,” Lawless says. “I choose moss. I’m 58 years old and I’m more active than most people with two legs. I live each day with the biggest smile I’ve got.”
AN INTERVIEW WITH THE DOCTOR
Dr. Allen Burton, Abbott’s medical director of neuromodulation and chronic pain therapies, spoke with PainPathways about the latest advances in the treatment of chronic pain.
Pain Pathways: What are some significant advances in chronic pain therapies at Abbott?
Dr. Burton: Neurostimulation—sending electrical signals to the brain to mask pain—has advanced dramatically in the last five years. Abbott’s understanding of neuroscience and how the body interprets pain has led to groundbreaking developments to treat chronic pain. We offer patients with many different pain conditions highly effective therapies called BurstDR stimulation and DRG stimulation through Abbott’s Proclaim platform. Both therapies draw on patient-centric design and functionality—for example, both use Apple iPod controllers. The comfortable nature of having a familiar technology to manage your chronic pain helps patients feel more like people who are managing their disease and living a full life.
PainPathways: What new developments are on the horizon that might be “game changers” for patients?
Burton: We are continually doing research on our neuromodulation technologies to improve their effectiveness and ability to continue to alleviate pain over the long term. Our BurstDR therapy happens to be the most studied novel waveform in the world. What this means to physicians and patients is that it is backed by clinical evidence and proven in the real world. A unique aspect to Abbott’s BurstDR stimulation is that it is designed to help patients find relief from their pain and suffering while also providing a better experience with chronic pain therapy. It’s truly a patient-centric technology, using Apple mobile devices as controllers and allowing patients to live their lives more fully.
It’s also worth noting that Abbott firmly believes that neuromodulation is part of the solution in America’s opioid crisis. Interventional therapies—such as BurstDR and DRG stimulation—are becoming even more important for patients suffering from chronic pain and who want a non-addictive alternative.
PainPathways: In terms of navigating pain treatment, where is the best place for patients to start when exploring options at Abbott?
Burton: Usually, we encourage potential patients to ask their doctor for a referral to an interventional pain specialist. In patients also seeing a pain specialist, we ask if they are a candidate for DRG therapy or BurstDR stimulation; both are exclusive therapies from Abbott. Also, help is available at Abbott.com or on Facebook.
PainPathways Magazine
PainPathways is the first, only and ultimate pain magazine. First published in spring 2008, PainPathways is the culmination of the vision of Richard L. Rauck, MD, to provide a shared resource for people living with and caring for others in pain. This quarterly resource not only provides in-depth information on current treatments, therapies and research studies but also connects people who live with pain, both personally and professionally.
View All By PainPathways