Dry Needling
When you hear the term “dry needling,” you may think it’s a kind of acupuncture. But the two therapies are, in fact, nothing alike, says Michael Coords, MD.
They both use needles and can help reduce pain, but even the needles are entirely different from one another.
Dry needling hasn’t been around as long as acupuncture, which Dr. Coords says “has been around since before bloodletting, since before we knew what the heart was or what blood was.” But dry needling isn’t entirely new, either.
The term “dry needling” is often credited to Janet Travell, MD. She wrote about it in the book she co-authored, Myofascial Pain and Dysfunction: Trigger Point Manual. (Volume one of the two-volume set was first published in 1983.) Travell, who was President John F. Kennedy’s personal physician, used the term “dry needling” to distinguish between two hypodermic-needle techniques used in trigger point therapy.
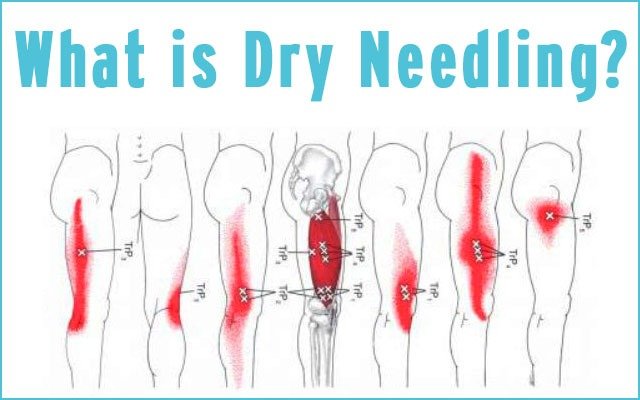
Dr. Coords, a musculoskeletal radiologist at the University of California—San Francisco, uses ultrasound to guide him when he’s performing fenestration, the medical term for dry needling. “I can see nerves and blood vessels,” he says. “I know where to place the needle—and it must be placed exactly where the pain is.
“The point is to create a response, to break something up,” he says. The needle induces an inflammatory response. For example, if you have a calcium buildup in a tendon in your rotator cuff—as did a patient I saw recently—the needle would poke the calcium, break it up, and the body would then absorb it.”
It’s worth noting that physical therapists perform dry needling, too, but the field is largely unregulated. The American Medical Association (AMA) stated in 2016 that the group “adopted a policy that said physical therapists and other non-physicians practicing dry needling should—at a minimum—have standards that are similar to the ones for training certification and continuing education that exists for acupuncture.”
The way Dr. Coords performs the procedure, it is an exact science—and science is the right word for it. It’s now a standard procedure and one with its own accepted diagnosis code. “Dry needling is science-backed medicine,” he says. “We perform this procedure for very specific reasons, and there’s just a small scope of reasons why we would perform it.”
Tendinitis is one reason. “I saw it, probably, 15 times today,” Dr. Coords says. He describes the condition as “a raggedy—but not torn—tendon.” If there is a tear in the tendon or muscle, it must only be a partial tear for dry needling to work.
Diagnosis is key
And here’s the main difference between dry needling vs acupuncture: your physician must know exactly what’s wrong with you to recommend and perform dry needling. You must have a diagnosis of something to know if it’s going to be right for you. Patients undiagnosed pain, Dr. Coords says—pain that still isn’t diagnosed even after it’s been treated, perhaps successfully.
While acupuncture works for many people, Dr. Coords treats a lot of patients who have tried acupuncture without success. One of his patients was a 35-year-old athletic woman. She had what he calls a “small cartilage defect” in her knee and treated it with acupuncture. Without a proper diagnosis, the problem worsened to the point that bone started rubbing against bone. She now needs a knee replacement—and she’s unusually young to need such a procedure. Had she gotten the correct diagnosis, Dr. Coords says, she could have been properly treated … without major surgery.
Dry needling can be highly effective for pain in the neck, shoulder, hip, knee and more, but whether a patient responds “rests largely on the underlying pathology,” Dr. Coords says. And the physician must know what he or she is doing: “Most patients fail when being treated by a physician who doesn’t understand what is wrong and what the limitations are.”
For instance, if a patient has a partial tear in her cartilage, dry needling can be an effective treatment. But a full tear? That requires surgery.
In 2000, Ariane, a West Hollywood–based food writer, chef and nutritionist, tried dry needling for her chronic shoulder pain. She was just 21 at the time and had tried a year of physical therapy; it hadn’t worked. She didn’t want painkillers, so dry needling was the logical next step recommended by her doctors.
Her first session was “moderately successful,” she says. She estimates it decreased her pain by about 10 percent. But during the second session, the first needle the doctor inserted struck a nerve. “I screamed for hours,” she says. “It’s the single most painful experience of my life to date, and it happened nearly 20 years ago.”
“They were shocked—and apologetic,” she recalls. She didn’t consider suing because it was “operator error,” not negligence. The answer to Ariane’s pain turned out to be acupuncture. “Acupuncture got rid of most of my chronic pain after dry needling failed,” she says.
It’s worth noting this happened two decades ago. Ariane’s story is a cautionary tale that bolsters Dr. Coords’ admonition: make sure your physician is using ultra-sound-guided dry needling.
Know what to expect
Patients need to know what to expect from dry needling. They’re not going to get immediate relief from it. In fact, they will likely hurt for one to two weeks after the procedure. “The point of the procedure is to cause local bleeding and inflammation,” Dr. Coords explains. “Within a couple of weeks, the body heals itself.”
Often, it takes just one session for a patient to see results. Dr. Coords has a follow-up phone call with his patients about two months after the procedure. Most report improved pain scores and better quality of life. If they don’t, Dr. Coords may recommend a second treatment.
Patients should not take any anti-inflammatory drugs after the procedure either—no Advil, Aleve or ibuprofen. The risks, he says, are the same risks you encounter any time you break the skin: “Assuming your doctor is using image-guided fenestration, then your risks are infection, bleeding and soreness.” If your doctor isn’t using ultrasound, Dr. Coords says, then the risks include damage to the cartilage, nerves and bones.
Massage: A Noninvasive Approach To Pain Management
Dr. Coords’ advice: know the risks. Get a proper medical diagnosis. Know what to expect. When it comes to treating pain, a needle is one weapon in the arsenal worth considering.
Needles—whether the kind used in dry needling or in acupuncture—aren’t the only answer to pain.
Less invasive methods can be highly effective. Most physicians recommend exhausting all other options before resorting to going under the knife. Or needle.
Massage may be just what the doctor ordered. First, be sure to understand the different forms of massage.
“Deep-tissue massage is the manipulation of soft tissue,” explains licensed massage therapist Mark Sears, who practices corrective massage. “Using slower, firmer pressure allows the tissue to give way to the much deeper layers of the muscles and fascia, which, in turn, allows for focus on muscular knots, trapped tension and discomfort.”
Don’t confuse deep-tissue massage with the kind of relaxing massage you might get at a spa. “Those have their place for people who are looking to de-stress or relax,” Sears says. “While deep-tissue [massage] is more for chronic pain and discomfort, a spa would use a much lighter touch.”
With deep-tissue massage, you might feel worse before you feel better. “After one deep-tissue massage, you can typically look to be sore for at least one to two days,” Sears says. “It’s just like a hard workout for the muscles. But the benefits may last around a week—or even more—depending on the client and the issue the therapist is trying to resolve.”
Don’t expect massage to be a once-and-done treatment. It should be regarded as ongoing maintenance. “I recommend regular maintenance massages,” Sears says. He likes to begin by seeing clients once a week for around eight to 12 weeks, depending on their condition. Then, he might drop back to every other week—but never less than once a month.
Massage helps with more than just sore muscles and relaxation, he says. “It has also been scientifically proven to help with cancer, HIV/AIDS, fibromyalgia, arthritis, and other chronic conditions.”
Dry needling vs acupuncture – or massage? What have you found to be the most beneficial? Comment below.
PainPathways Magazine
PainPathways is the first, only and ultimate pain magazine. First published in spring 2008, PainPathways is the culmination of the vision of Richard L. Rauck, MD, to provide a shared resource for people living with and caring for others in pain. This quarterly resource not only provides in-depth information on current treatments, therapies and research studies but also connects people who live with pain, both personally and professionally.
View All By PainPathways