Postherpetic Neuralgia
NO ONE BELIEVED HER,
In the following weeks, Schrader was tossed from doctor to doctor, with no explanation for why her bloodshot, watering eye hurt so badly that she could hardly bear to keep it open. Finally, a month after her symptoms first appeared, the sixth ophthalmologist to examine her saw a hazy spot on the back of her eye, which was identified as scar tissue on a nerve, caused by shingles. Unfortunately, this observation did not bring Schrader much relief. By now she was suffering from such severe pain that she received a new diagnosis: postherpetic neuralgia (PHN).
The ORIGINS of a PHN DIAGNOSIS
Simply stated, PHN is a painful complication of shingles. Shingles itself is caused by the varicella zoster virus, the same virus that causes chicken pox. After chickenpox re-solves, the virus goes into hiding in the nerve tissue near the spinal cord and brain. Later, due to either advanced age or a weakened immune system, the virus can reappear in the form of shingles. The result is an itchy, raised rash with a band of blisters that typically wraps around one side of the chest from the spine to the front. The shingles rash also can form on one side of the neck, face or head or around one eye. Typically, shingles begins with intense pain in the area where the rash later develops. Blisters may emerge within a few days after the initial pain is felt, then crust over and disappear within a few weeks.
However, for some patients this is the beginning, not the end, of a painful journey. The pain from PHN is caused by nerve damage resulting from the shingles virus, eliminating the ability of the brain and affected area to com-municate properly. If the pain lasts more than a monthafter the shingles blisters have healed and no other reasonfor the pain can be found, a diagnosis of PHNis made.
WHO’S at RISK?
According to Porter McRoberts, MD, a pain specialist in Fort Lauderdale, Florida, about 10–20 percent of those with shingles will develop PHN, and most of those patients recover quickly. Only 7 percent have pain at 3months, a figure that drops to 4 percent at a year. Some patients, however, experience chronic pain from PHN longer, even for a lifetime.
PHN occurs most commonly in the elderly. Those younger than 50 have a very low incidence of the condition. “Studies show that as age increases so, too, does the likelihood of developing PHN,” says Dr. McRoberts.
The PAIN and SUFFERING of PHN PATIENTS
The symptoms of PHN include pain classified as burning, jabbing, gnawing, sharp or aching. Often, PHN patients cannot bear to have anything, even clothing, touch the affected area. Less commonly, patients experience itching, numbness, weakness or paralysis. Ted Stout, who has had PHN for ten years, experiences stabbing pain on the left side of his forehead. He also battles chronic fatigue, a commonly reported symptom of PHN.
“At the pain’s worst I feel as though I just had surgery,” says Stout. “It’s always a stabbing headache.”
Schrader is frustrated by her pain, too, saying that when the pain flares, it feels as if an ice pick is constantly being driven into her eye. Both Stout and Schrader claim that stress —or any sort of emotional trigger—makes their pain worse, as does lack of sleep.
PREVENTION is the BEST MEDICINE
Medical experts agree that prevention is the most effective way to stop the onset of PHN. In 2006, a vaccine called Zostavax that reduces the risk of shingles was licensed and released to the public. It is recommended for people 60yearsand older, and while it doesn’t provide complete immunity from shingles, it does reduce the severity and possible complications.
“I recommend the Zostavax vaccine to all of my patients above the age of 60,” says Jacques Laguerre, MD, a family medicine physician in Monroe, North Carolina. “Primary prevention is always the best medicine.”
Dr. McRoberts adds that the vaccine halves the risk of developing shingles and appears to shorten the associated painful period as well. “Interestingly, in those older than70 who do develop shingles, the vaccine seems to reduce the frequency of PHN,” he says.
While most people in the U.S. are given the chicken pox vaccine (varicella vaccine) as babies, experts recommend thatadults and older children who have never had chicken pox receive the varicella vaccine to reduce the risk of catching the virus.
For those who develop shingles, the Mayo Clinic’s website indicates that when antiviral medications, such as Acyclovir, are started within 72 hours of the onset of symptoms, the risk of developing PHN is reduced by 50 percent.
“The antiviral medications reduce the severity and duration of the viral infection and also lessen the duration and severity of shingles,” says Dr. McRoberts. There is no evidence yet that links the use of antiviral medications to decreased incidence and severity of PHN. However, one can speculate that if antiviral medications prevented shingles from ever occurring, then PHN would never develop.
PHN’S BIGGEST CHALLENGE is EFFECTIVE TREATMENT
Even though PHN is easy to diagnose, it is notoriously difficult to treat.
“Since the pain is from injury to the nerve itself, many of the more common treatments like anti-inflammatories and opioids don’t work as well for PHN as they do on other types of pain,” Dr. McRoberts says.
Several years ago, the Agency for Healthcare Research and Quality (AHRQ) released guidelines regarding the treatment of PHN. AHRQ’s research revealed certain medications effective in treating PHN, including tricyclic antidepressants, gabapentin, pregabalin, opioids and topical treatments, such as lidocaine patches, aspirin cream and capsaicin. Antidepressants are thought to work because they affect the brain chemicals norepinephrine and serotonin, which impact how the body interprets pain. It is believed that antidepressants do not eliminate the pain but instead make it more tolerable. Anticonvulsants, such as gabapentin and pregabalin, are most often prescribed for seizure control. However, in the case of PHN, they are effective in their ability to “calm” the injured nerves by stabilizing abnormal electrical activity. According to the International Association for the Study of Pain (IASP), topical treatments such as lidocaine patches are shown to be effective as a first line of defense against PHN and can help eliminate pain when used with other treatments.
Since many patients who develop PHN are older adults, doctors must take special care in determining their medication dosages, as these patients cannot always handle the high doses of medications required to produce effective results. “Treatment options can be limited in the elderly because of the doses needed to effectively treat PHN,” says Dr. Laguerre. “These medications can have some intolerable side effects, including hypersomnolence [excessive sleepiness] and gait instability.”
Patients should review all medications with their primary care physicians so cross-interactions and side effects can be appropriately managed.
ATTACKING PHN with a ONE-TWO PUNCH
“Often, several approaches at once treat PHN the best,and just because one therapy isn’t working doesn’t mean you should immediately abandon it for another,” says Dr. McRoberts. “This is because the concomitant use of several approaches often provides the best overall treatment.”
No one knows this better than Schrader, who received countless prescriptions before she found the right regimen, combining OxyIR and OxyContin. But with that came a stigma that taking these powerful medications may lead to addiction.
“None of my family members understood,” says Schrader, recalling their assumption that she might become addicted to the medications. “I thought I was losing my mind. It almost ruined my relationship with my boyfriend. He started thinking I was an addict.”
However, Schrader was able to function at work with low doses of OxyIR, and her employer was aware of her condition and medications. When not at work, Schrader takes OxyContin. When she became pregnant last year, all of her symptoms improved, but several weeks after the baby was born, her eye pain returned and so did her need for prescription pain medications.
Stout takes a regimen of pregabalin, antidepressants and opioids and has made several lifestyle changes to make living with PHN tolerable.
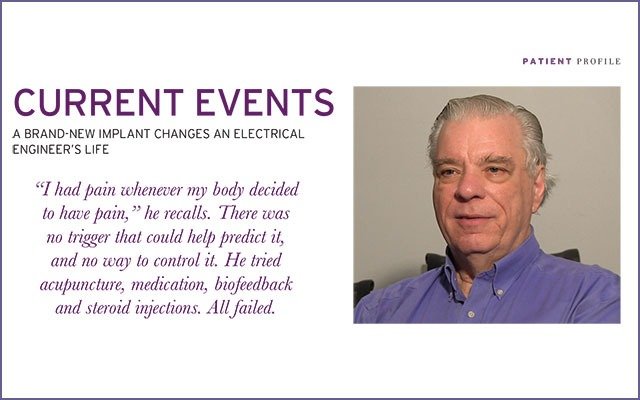
When the pain from PHN does not respond to conventional approaches, such as medications and lifestyle changes, more aggressive treatments are available, including spinal cord and peripheral nerve stimulation. Dr. McRoberts points out, though, that there is limited scientific evidence to show that these treatments are clearly beneficial or effective. However, they may be helpful as a last resort.
Dr. McRoberts recommends patients see their primary care physicians when managing pain from shingles, but if they develop PHN, patients should seek care from a pain specialist.
SUPPORT for PHN
When Schrader developed PHN, she felt that no one understood what she was enduring, so she created a support group on Facebook: Postherpectic Neuralgia (PHN)/Chronic Neuralgia Support Group. Stout and many others have joined that group, creating a forum where remedies, success stories and failed treatments can be shared. When asked what advice Schrader would offer to other PHN sufferers, she stresses the importance of seeking a second opinion and not stopping until an effective treatment plan has been created. She also wants PHN patients to know they are not alone. In the past, she says, she suffered from bouts of depression, feeling as if no one understood her ordeal. Thankfully, through her online support group, Schrader no longer feels this way. Likewise, Stout encourages PHN patients to stay strong and not get discouraged.
“Until a year ago I was ready to retire on disability,” says Stout. “Now, through some changes in medications and chiropractic care, I am 50 percent better.”
For Stout, and others with PHN, every improvement in chronic pain management is a major milestone.
PainPathways Magazine
PainPathways is the first, only and ultimate pain magazine. First published in spring 2008, PainPathways is the culmination of the vision of Richard L. Rauck, MD, to provide a shared resource for people living with and caring for others in pain. This quarterly resource not only provides in-depth information on current treatments, therapies and research studies but also connects people who live with pain, both personally and professionally.
View All By PainPathways




I have PHN also. Recently I came across research that has been done on high dose Vitamin C infusion therapy. I had it done at a local IV infusion salon with really good promising results. I am on the FB group Post herpetic neuralgia (PHN)/Chronic neuralgia support group and posted my experience there.
I just don’t know why this isn’t more widely known in the pain management practices of physicians that help manage this disease.