Understanding Hiatal Hernia: Diagnosis, Treatment, and Dietary Considerations
In the realm of digestive disorders, a hiatal hernia is a condition that often goes unnoticed until it manifests with uncomfortable symptoms. As the medical community continues to evolve and standardize diagnostic codes, the ICD-10 (International Classification of Diseases, 10th Revision) has become a crucial tool for accurately identifying and documenting various health conditions, including hiatal hernia.
ICD-10 and Hiatal Hernia
The ICD-10 is a comprehensive system used by healthcare professionals worldwide to classify and code diseases, injuries, and other health-related conditions. Within this system, hiatal hernia is classified under the code K44, which encompasses various types of hernias, including diaphragmatic hernias.
Specifically, the ICD-10 code for hiatal hernia is K44.9, which refers to a hernia of the diaphragm without any further specification or complication. In some cases, additional codes may be used to provide more detailed information about the type of hiatal hernia or any associated complications.
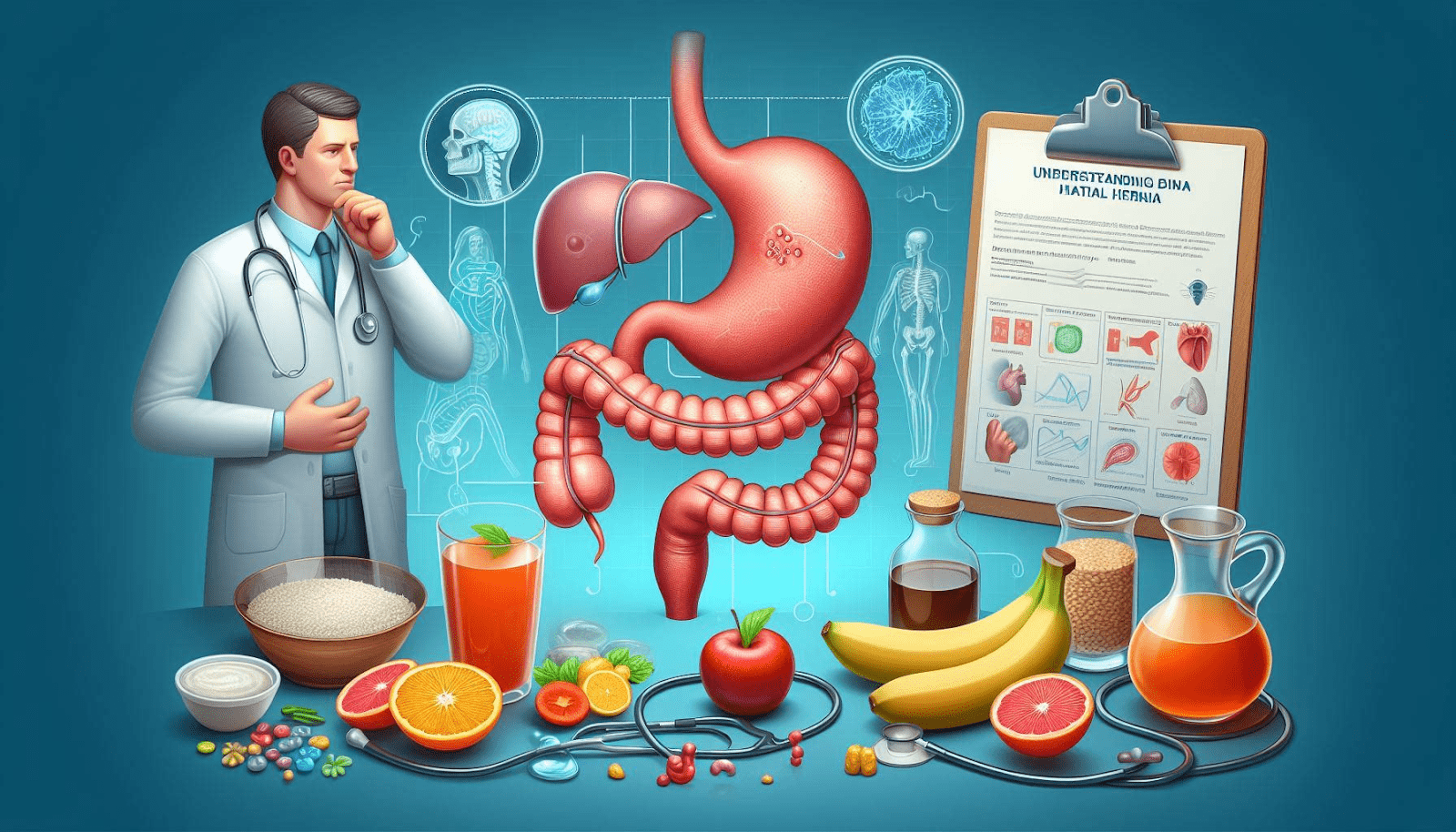
Understanding Hiatal Hernia
A hiatal hernia occurs when part of the stomach protrudes through the hiatus, an opening in the diaphragm muscle that allows the esophagus to pass through from the chest cavity into the abdomen. This protrusion can result in various symptoms, such as heartburn, regurgitation, difficulty swallowing, chest pain, and a feeling of fullness or discomfort in the upper abdomen.
There are two main types of hiatal hernias:
1. Sliding hiatal hernia: This is the most common type, where a portion of the stomach and the gastroesophageal junction (the area where the esophagus meets the stomach) slide up through the hiatus into the chest cavity.
2. Paraesophageal hiatal hernia: In this less common type, part of the stomach bulges through the hiatus, but the gastroesophageal junction remains in its proper place.
While hiatal hernias are often asymptomatic, they can sometimes lead to complications such as gastroesophageal reflux disease (GERD), erosion or ulceration of the stomach lining, and even strangulation of the herniated portion of the stomach (a medical emergency).
Treatment Options for Hiatal Hernia
The treatment approach for hiatal hernia depends on the severity of symptoms and the presence of any complications. In mild cases, lifestyle modifications and medication may be recommended:
1. Lifestyle changes: Losing weight (if overweight), avoiding tight clothing, quitting smoking, and elevating the head of the bed can help reduce symptoms.
2. Medications: Over-the-counter or prescription medications, such as antacids, H2 blockers, or proton pump inhibitors, may be prescribed to manage acid reflux and heartburn.
In more severe cases, or when lifestyle changes and medications fail to provide adequate relief, surgical intervention may be recommended. The most common surgical procedure for hiatal hernia is called a Nissen fundoplication, which involves wrapping the upper part of the stomach around the lower esophagus to reinforce the valve between the stomach and esophagus.
Dietary Considerations After Hiatal Hernia Surgery
While hiatal hernia surgery can effectively alleviate symptoms and prevent complications, proper post-operative care is crucial for a successful recovery. One important aspect of this recovery process is adhering to dietary guidelines, which may include specific food restrictions.
One such restriction that patients often encounter after hiatal hernia surgery is the recommendation to avoid chocolate. But ‘why no chocolate after hiatal hernia surgery’?
The rationale behind this dietary advice lies in the potential impact of chocolate on the digestive system and its ability to exacerbate symptoms related to hiatal hernia. Here are some reasons why chocolate may be discouraged after hiatal hernia surgery:
1. Chocolate and acid reflux: Chocolate contains compounds called methylxanthines, which can relax the lower esophageal sphincter (LES), the muscle that acts as a barrier between the esophagus and stomach. When the LES is relaxed, it can increase the risk of acid reflux and worsen symptoms associated with hiatal hernia.
2. Caffeine content: Many types of chocolate contain caffeine, a stimulant that can further relax the LES and increase the production of stomach acid, potentially leading to heartburn and discomfort.
3. Fat content: Chocolate, particularly milk and dark varieties, is high in fat. Consuming fatty foods can delay stomach emptying, increasing the risk of acid reflux and discomfort in individuals with hiatal hernia.
4. Potential irritation: The compounds and additives found in chocolate may act as irritants to the delicate tissues of the esophagus and stomach, potentially exacerbating symptoms in some individuals.
It’s important to note that while chocolate is often restricted after hiatal hernia surgery, the duration and extent of this restriction may vary depending on the individual’s recovery progress and the specific recommendations of their healthcare provider.
In addition to avoiding chocolate, patients may also be advised to limit or avoid other foods and beverages that can potentially trigger or worsen reflux symptoms, such as spicy, fried, or acidic foods, as well as alcohol and caffeinated beverages.
Conclusion
Hiatal hernia is a digestive condition that requires proper diagnosis, treatment, and post-operative care to manage symptoms and prevent complications. The ICD-10 coding system plays a crucial role in accurately identifying and documenting this condition, enabling healthcare professionals to provide appropriate care.
While surgical intervention may be necessary in severe cases, dietary modifications, including the avoidance of certain foods like chocolate, are often recommended to support recovery and prevent symptom recurrence. By adhering to these dietary guidelines and maintaining open communication with healthcare providers, individuals with hiatal hernia can effectively manage their condition and improve their overall quality of life.
Remember, ‘why no chocolate after hiatal hernia surgery’ is not a whimsical restriction but rather a strategic measure to minimize the risk of acid reflux, discomfort, and potential complications during the recovery process. Embracing these dietary recommendations, along with other lifestyle modifications and medical treatments, can pave the way for a successful journey toward better digestive health and well-being.
Dr. Elizabeth Novello
Dr. Elizabeth Novello is a distinguished healthcare professional who has dedicated her career to the specialized field of pain-related healthcare. With a deep passion for alleviating suffering and improving the quality of life for those experiencing pain, Dr. Novello has become a recognized authority in her field. Dr. Novello’s journey in the realm of pain management began with her rigorous medical training, where she developed a profound understanding of the complexities surrounding pain and its treatment.
View All By Dr. Elizabeth