Sexual Pain
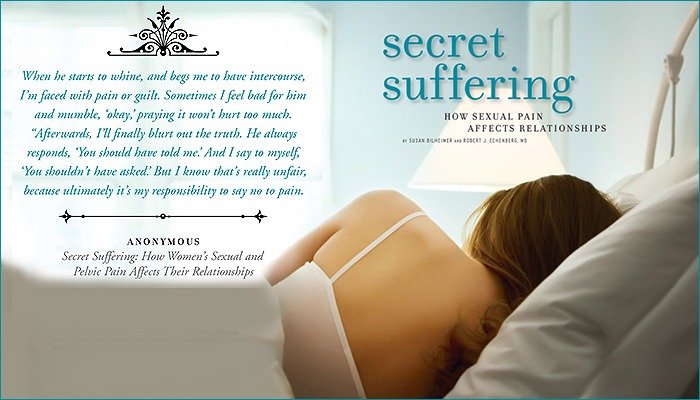
Sex hurts. That’s the bottom line for millions of women. Although there’s a tremendous stigma associated with sexual pain, it is a devastating component of a debilitating condition called chronic pelvic pain (CPP). According to the International Pelvic Pain Society (IPPS), CPP is one of the most common medical problems affecting women aged 18 to 50 today. Close to 20 million American women have CPP, with 90 percent suffering from sexual pain.
According to the IPPS, over half of these sufferers have not been properly diagnosed. The stress that stems from not being properly diagnosed is difficult enough. But when women in pain are also intimately involved, their suffering can threaten even the best of relationships.
Some women describe sexual pain as a stabbing, searing, cutting or burning sensation during vaginal penetration. Others say that a touch on their clitoris or vulva sends them into sharp, piercing spasms. Still others talk about the throbbing, raw feeling that may follow for hours or days after intercourse. Many describe a pressure to urinate that makes them feel their bladder will explode during and after sex.
Women who may also have irritable bowel syndrome (IBS) say that constipation makes intercourse feel like a sword is stabbing their intestines.
Far too many women are ashamed to discuss their sexual pain, even with their partner. Instead, they suffer in silence and engage in sexual acts that cause them in-tense discomfort. When they do attempt to find help, women often confront a medical community intent on convincing them the problem is “in their head,” when in fact the issue is often a lack of education on the part of health care providers and an unwillingness to spend the time required to treat these patients.
THE PUDENDAL NERVE’S ROLE IN PELVIC AND SEXUAL PAIN DISORDERS
One cause of sexual pain gaining more attention is pudendal neuralgia. Robert J. Echenberg, MD, gynecologist in Bethlehem, Pennsylvania, and leading expert on sexual and pelvic pain, describes the pudendal nerve as a key component in providing sensations that range from pleasure to pain. Pudendal neuralgia is a neuropathic pain condition involving inflammation and dysfunctional firing of the pudendal nerve. The pudendal nerve can become sensitized and send out pain signals to the genitals and associated systems due to physical/emotional injury, nerve entrapment, surgery or other trauma.1 As shown in the illustrations on page 63, branches from the pudendal nerve connect directly with the sexual organs and tissues, such as the clitoris, labia, vulva, anus and perineum (tissue between the vaginal opening and anus).
OTHER SEXUAL PAIN SYNDROMES LINKED TO THE PUDENDAL NERVE
Many sexual pain syndromes can be triggered by pudendal neuralgia. For instance, with generalized vulvar pain (vulvodynia), pain signals transmitted from the pudendals may cause women to experience discomfort with the slightest pressure (such as from sitting or wearing pants), or even with no pressure at all. The pudendal nerve also connects to the vestibule (tissue at the opening of and leading into the vagina). According to Dr. Echenberg, vestibulodynia (irritation of the vestibule) is, by far, the most common reason for pain upon sexual penetration or insertion of tampons in reproductive-aged women. This condition is frequently misdiagnosed and treated as a vaginal infection.
PELVIC FLOOR DYSFUNCTION
When pelvic pain becomes chronic, there’s a corresponding spasm or contraction of the surrounding pelvic floor and sidewall muscles. This condition is called pelvic floor dysfunction (PFD). Dr. Echenberg states that PFD is almost always found in women with CPP and, as he describes, “Eventually, a vicious cycle begins in which the nerves fire off through the pudendal because of previous injuries, surgeries, pelvic organ dysfunctions and sometimes emotional pain imprinting,2 and the muscles respond by contracting throughout the pelvis.”
HOW TO COPE
Managing your life when you suffer with sexual pain can be challenging. But there are steps you can take to regain intimacy with your partner, find relief from your symptoms and work toward getting a proper diagnosis and treatment.
WHAT YOU CAN DO
1) Speak out. Become an advocate for yourself in andout of the bedroom. Staying silent will only make you feel more alone and powerless.
2) Don’t ignore it. Pain is a signal. Seek help early and keep searching for answers until you get them.
3) Educate yourself. Talk to others who share your diagnosis and symptoms. Find reputable sources for information. (See sidebars on pages 64 and 65.) Knowledge is power when you walk into a doctor’s office.
4) Acceptance is sometimes the best course. Fighting the reality of your situation may not be productive. Relief often comes when you work to cope with your chronic condition rather than try to cure it.
TREATMENT
Dr. Echenberg stresses that a nonsurgical approach is the most effective when pain is the primary diagnosis. Multi-modality therapies, such as medication and pelvic floor physical therapy, are essential to:
1) Control the “triggers” of pain (e.g., painful bladder syndrome, irritable bowel syndrome, endometriosis)
2) Control nerve pain itself, and
3) Relax the resulting severe muscle spasms with specialized physical therapy techniques or similar treatment.
HOW TO WORK EFFECTIVELY WITH YOUR DOCTOR
1) Be proactive. Ask questions. Speak up, especially if you feel you aren’t being heard. Tell your doctor if you have symptoms such as frequent urination and/or sexual pain, and no infection.
2) Get all appropriate tests to rule out acute and/or chronic diseases. After that, get down to the task of management with your doctor.
3) Manage, not cure. If you hear the word “cure” regarding your chronic condition, be wary.
4) Partner with your doctor. Learn all you can about your condition. Don’t be afraid or intimidated to bring information to him or her. A good health care provider wants to learn more to help you.
5) Work with a pelvic floor physical therapist (PT). Most doctors knowledgeable about CPP consider this a core treatment component. You’d go to physical therapy for other types of muscle spasms and injuries, and in this case, PTs can help train you to relax your pelvic floor muscles.
6) Locate an understanding doctor. Many women find tremendous relief by having a doctor who will listen and validate their pain. Find another doctor if yours rushes or belittles you, or implies that your pain is not real.
7) Doctors can check. It’s easy for doctors to check for pudendal sensitivity by pressing one finger on each side of the pelvis near the bony prominence on which you sit. Many patients have tenderness on one or both sides, precisely where the pudendal nerve exits from its tiny canal and branches out into the entire vulvar region. This simple test alone might save women countless false diagnoses.
HOW TO IMPROVE YOUR RELATIONSHIP WITH YOUR PARTNER
1) Say NO to pain. Stop giving in to painful sex out of guilt or fear that your partner will leave or cheat on you. If you associate sex with pain, eventually you will become resentful and react in some way. The sports adage “No pain, no gain” is definitely not applicable to sex.
2) Say YES to shifting your thinking about sex. If water is soothing, then have sex in the shower. If intercourse hurts, explore other ways to be sexually aroused, such as manual simulation, oral sex or the use of a vibrator. One thing is certain: to overcome sexual obstacles with your partner you need to shed inhibitions and to be willing to experiment. Opening your mind can make all the difference in whether your relationship can withstand the trials you may go through with your condition. A willingness to try new forms of pleasure can rekindle sexuality in a new and exciting way.
3) Intercourse is not sex — it’s a sexual act. Some think intercourse is the only “real” sex. Couples should embrace new methods and try new tech niques to enhance their sexual experiences.
4) Schedule a weekly date. See a movie, go to a museum, visit the planetarium. Afterwards, spend some time getting physically close to each other, even if it doesn’t culminate in sex. Experiment with pain-free forms of sexual pleasure together. Even if you are in too much pain for sexual activity, your partner could give you a back rub after you sexually satisfy him or her in a way that causes you no dis-comfort.
5) Talk to your partner about your condition. Give your partner a chance to help you by inviting him or her to go to the doctor with you. Intimacy is strengthened when two people work together to solve a problem.
6) Be patient. It may take some time, creativity and determination to change the situation. But it’s worth the effort to restore pleasure and intimacy to your life. {PP}
1. Over one’s lifetime there is an unconscious laying down of a chemical “memory” into the central nervous system of every physical and emotional pain that one experiences.
2. The nervous system has cumulatively stored memories of traumatic events throughout one’s life, such as physical and/or emotional injuries, abuse, surgeries, intensive sports activities, and so forth. These are all part of an individual’s past history and provide a guidebook to the nervous system as to how to interpret events that are happening right now. Our nervous system uses this information to not only determine whether you feel pain, but how, when, and where the pain shows up based on what is going on in the body at the time. “The problem is that for some people, these accumulated traumas and experiences may result in a condition called ‘central sensitization,’ which means the central nervous system [CNS, the brain and spinal cord] sends out pain signals in reaction to even small amounts of stimuli,” said Dr. Echenberg. From “Secret Suffering”
PainPathways Magazine
PainPathways is the first, only and ultimate pain magazine. First published in spring 2008, PainPathways is the culmination of the vision of Richard L. Rauck, MD, to provide a shared resource for people living with and caring for others in pain. This quarterly resource not only provides in-depth information on current treatments, therapies and research studies but also connects people who live with pain, both personally and professionally.
View All By PainPathways